By Tina Payne Bryson, LCSW, PhD
At the Center for Connection, our interdisciplinary approach allows us to paint with a broad brush when working with clients and supporting them in their goals. For example, in a case where the client presents with ADHD and depression, a frequent recommendation might be to recommend Dialectical Behavior Therapy (DBT). However, at the CFC, we might view this client's needs differently and consider more “bottom up” and “top down” strategies.
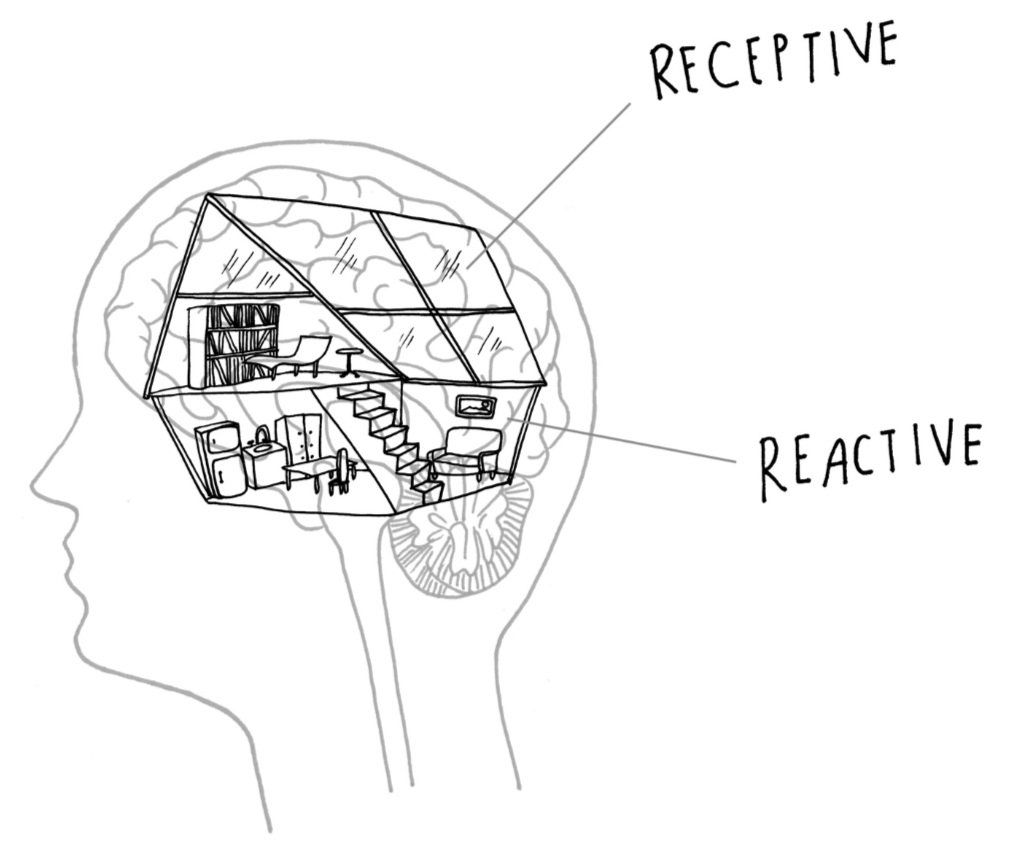
Regulation vs. Dysregulation
When we’re regulated and able to think and consider, we can use “top down” strategies like pausing before action, noticing and deciding, self-talk, talking about feelings, and problem-solving.
When we’re dysregulated, we can’t do those things well at all, so we need “bottom up” strategies that regulate our nervous systems to allow us to get back into an integrated brain where we can use "top down" strategies as well (such as DBT).
General Bottom Up Strategies
Some of the best "bottom up" strategies are:
Co-Regulation (which is when someone is connecting with you to comfort and get you back to regulation through their presence)
Sensory-Based or Body-Based approaches
For example, the “physiologic sigh” which is when your exhale is longer than your inhale and which is very powerful to down-regulate your nervous system.
Sensory inputs that are regulating
Movement
Breathing in a specific way
And more
General Top Down Strategies
General “top down” strategies can include teaching clients to use
Dialectical Behavior Therapy (DBT)
Cognitive Behavioral Therapy (CB)
Mindful Noticing
Naming Feelings
Curiously becoming insightful about a behavior we might have
Role playing how to handle situations better in the future
And more
In these examples, we’re working with the brain’s plasticity and giving “reps” to the prefrontal cortex.
Therapeutic Bottom Up Strategies that Support Top Down Approaches
In therapy at the CFC, we do a lot of both.
When we use top down strategies, we’re giving repeated opportunities for the prefrontal cortex to practice. And that part of the brain is built from lots of things, including development unfolding, but also through things we can support:
1. Through providing safe, positive, predictable relationships throughout development, (including that with the therapist); and,
2. through repeated experiences that flex and use that part of the brain.
In our example above, we know that kids with ADHD have a quick “gas” for emotional and behavioral impulsivity (without strong “breaks”) and need lots of reps to build this part of the brain.
We also work with clients on bottom up strategies so that when they’re in intense emotional states, dysregulated, etc., they have strategies they can use to regulate their nervous systems so they can get back to pausing, making decisions, etc. This is especially important because while top down can prevent that “flipped-lid” state, once it’s there, top down strategies are inaccessible and our client needs to get in the reps on regulation from the bottom up, too.
From there we can work toward what I wrote about with Dr. Dan Siegel in The Whole-Brain Child to create integration in the brain. This happens when bottom up and top down approaches to come together to help kids be more Flexible, Adaptive, Coherent (doing what makes sense), Energized (not depressed), and Stable.
A handy way to remember this is to think of the “FACES” of an Integrated Brain:
We can also collaborate with other professionals, like psychiatrists where meds can support our client or by working with OTs to help turn the dial down on sensory processing, or focus on other pieces that are an important part of the picture.
Considering all of these tools and approaches, we can see that some of the depression (in our case study above) may be a result of the gap between what the child wants and what he’s able to do, given his challenges, followed by him then feeling bad and angry about/at himself. And when we use DBT, we know a lot of it is about reframing how you see things, so that “mindsight” and self-attunement may be helpful as well, and so are lots of other approaches.